COPD
Diagnosis
Consider COPD in smokers aged over 40 years with recurrent antibiotics for chest infections. Other risk factors include occupational exposure and alpha-1 antitrypsin deficiency
Presenting with symptoms of progressive dyspnoea, chronic productive cough, and wheeze
Diagnose with post-bronchodilator spirometry: FEV1/FVC < 70% with progressive respiratory symptoms is diagnostic of COPD, though may under-diagnose in women and younger patients
Assess for co-morbid asthma? diurnal variation, atopy, bronchodilator reversibility > 12% implies element of asthma
WHO Suggests Alpha-1 Antitrypsin levels in all new diagnoses
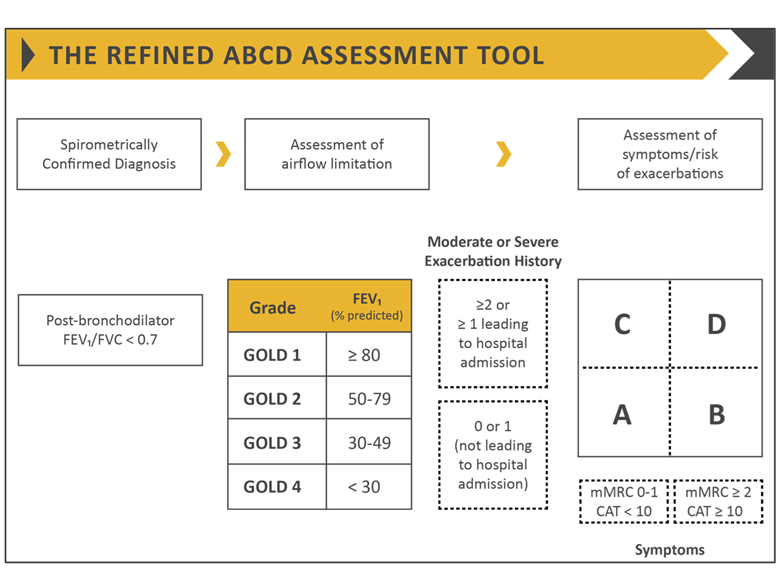
Grading
GOLD Modified ABCD assessment Tool - patients get a numerical grade and letter category. The number quantifies degree of airflow limitation, the letter assesses exacerbation frequency and functional limitation.
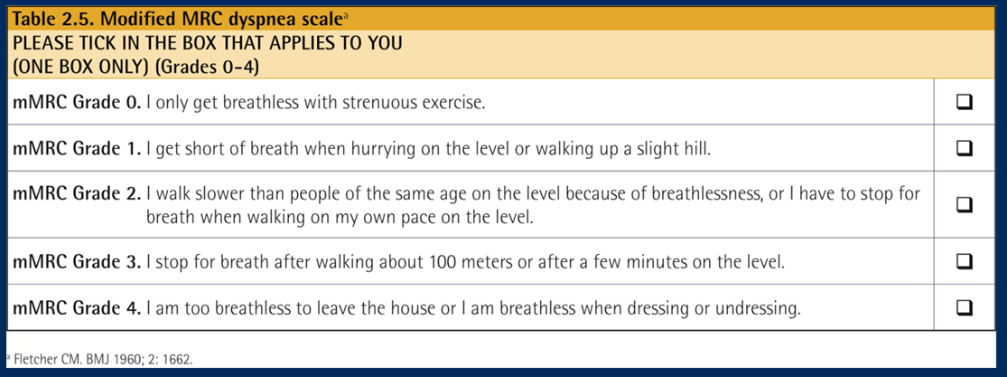
 Modified MRC Dyspnoea Scale
Modified MRC Dyspnoea Scale
COPD Assessment Test (CAT) - measures impact of symptoms on QOL
Management
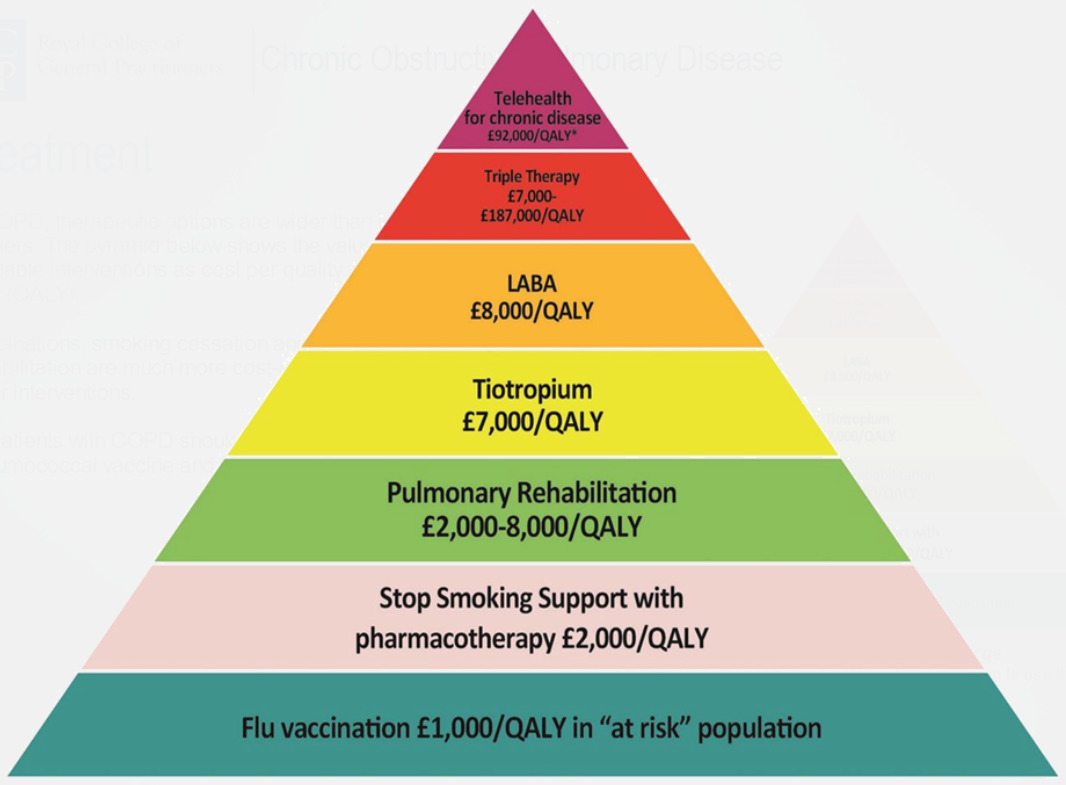
Smoking Cessation
Smoking cessation slows rate of decline in FEV1
Start prescription two weeks before chosen stop date
- Nicotine Replacement Therapy: 8-12 weeks, then slow taper over up to 9 months
- Bupropion: 7-9 weeks, not in pregnancy, c.i. in seizure disorder
- Varenicline: 12+12 weeks, not in pregnancy, previous suspected links with suicidality/depression, current evidence suggests no reason to withhold from patients with mental health issues
Pulmonary Rehabilitation
- Programme of physical exercise and information
- Improves dyspnoea, health status, and exercise tolerance
- Should be started within four weeks of an acute hospital admission
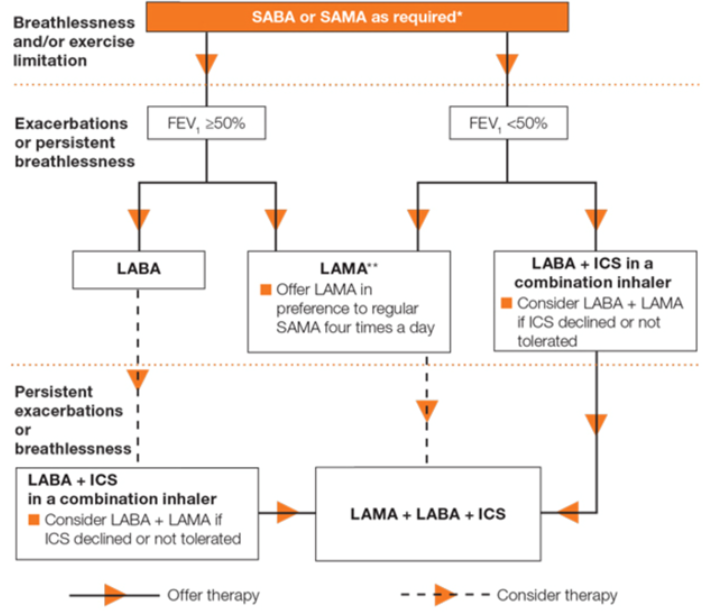
NICE Algorithm
GOLD Algorithm
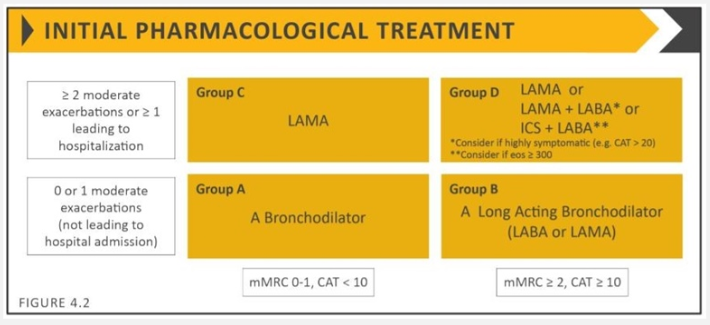
Key points:
- LAMA superior to LABA in exacerbation prevention
- Prolonged ICS use increases pneumonia risk - therefore LABA/LAMA preferable to LAMA+ICS in patients with recurrent exacerbations
- Before escalation review inhaler technique and adherence
- Also prescribe 'rescue' pack of oral antibiotics and steroids for exacerbations
If insufficient, consider:
- Roflumilast - Oral PDE4 inhibitor; given if FEV1<50% and admission in previous year; a secondary care drug
- Macrolide (ie azithromycin) od or 3x/week to reduce exacerbation frequency
- Consider ICS cessation as increases risk of pneumonia (see guideline)
Home Oxygen
Indication for referral
- SpO2 <= 92%
- FEV1 < 30%
- Cyanosis
- Secondary polycythaemia
- Peripheral oedema
- Raised JVP
Symptomatic Treatment
- Dyspnoea
- Opioids
- Fans
- Neuromuscular electrical stimulation
- Chest Wall Vibration
- Pulmonary Rehabilitation
- Mucus
- Carbocysteine
- NAC
- Nutritional Support